Prior Authorization and Medical Policies
AZ Blue uses the prior authorization review process to determine your eligibility for a requested procedure or medication before you receive it. It’s not a guarantee of payment.
Our clinical staff (doctors and nurses) make authorization decisions on your eligibility, health condition, the specific benefits in your plan, and the clinical guidelines to determine if the recommended care is medically necessary for your situation.
Note: The fact that a provider has prescribed, ordered, or recommended a service for you does not make it medically necessary or make the service eligible for your Medicare Advantage health plan benefits, even though it may not be expressly excluded in your Evidence of Coverage. Even if a service is authorized, we still review the claim and process it according to your plan coverage, including any limitations, exclusions, maximums, and waivers.
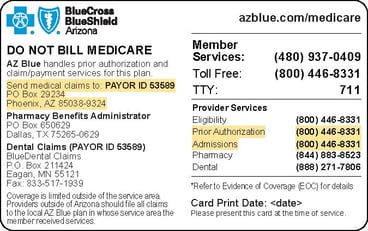
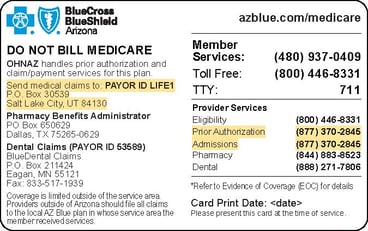
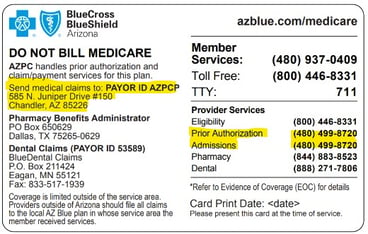
To find the prior authorization requirements for your plan, first check the back of your ID card. It will look like one of the three samples below. The name you see in yellow highlight on the left side of your card is who will take care of prior authorizations you might need for certain services. You can call the prior authorization number on your card, for more information or view the prior authorization lists in the links below. You can also ask your healthcare provider to check if prior authorization is needed for a recommended service or medicine.
- AZ Blue: 1-800-446-8331 | AZ Blue Prior Authorization List
- Optum Health Network Arizona (OHNAZ): 1-877-370-2845 | Optum Prior Authorization List
- Arizona Priority Care: 480-499-8720 | Arizona Priority Care Prior Authorization List
If you are admitted for inpatient care, your provider must inform us within 24 hours or the next business day. Prior authorization may also be required for scheduled inpatient care.
- AZ Blue: 1-800-446-8331 | AZ Blue Prior Authorization List
We use medical policies to guide our decisions on prior authorizations and claims. Our policies are based on evidence-based clinical research. We carefully review new healthcare technology and scientific findings as they become available.
For your Medicare Advantage plan, we use the following medical policies:
- CMS National Coverage Determinations (NCD)
- Local Coverage Determinations (LCD)
- EviCore Guidelines
- MCG Care Guidelines, please call 1-800-446-8331.
- Part B Step Therapy Drug List and Criteria
- Medicare Advantage Ambulance Services
- Davis Vision Guidelines
- American Specialty Health (ASH) Guidelines
- Arizona Priority Care (AZPC) Guidelines
- OptumCare (OHNAZ) Guidelines
Note: If you can’t find what you’re looking for, please call us at 1-800-446-8331 TTY: 711.